The patient of geriatric nurse Katharina Schmidt is whimpering in pain. The 82-year-old has fallen on an icy road and sustained multiple fractures to his upper arm. After lying in hospital for a long time and then at home, painful pressure points form on his buttocks, which open up after a short time. Repositioning and the right aids remain essential – the senior needs to be moved. However, many aids and methods for pressure injury prevention are outdated.
Why is individual therapy crucial?
Every patient needs a customized approach. There is no such thing as an universal aid. The factors can be divided into two categories: Intrinsic and extrinsic risks. Intrinsic risks include physical condition, underlying diseases, age, overweight or underweight, mobility status or malnutrition. Extrinsic factors include the positioning of the patient, catheters or probes, medication, bandages or restraints and surfaces that are too hard. Patrick Kolb, spokesperson for the Decubitus Forum in the German Medical Technology Association (BVMed) from Berlin, emphasizes in an online interview „that the focus must be on the individuality of each patient“.
How have storage intervals changed?
A rigid change every two hours used to be the standard. Modern approaches take individual needs into account. A doctor should be consulted at the first signs of a pressure ulcer, such as persistent pain or reddened skin on a particular part of the body. One indicator is the finger method. This involves pressing with the finger on redness, for example on bony prominences. If the skin remains red, the patient must be repositioned immediately and the intervals between changes shortened.

Another modern solution is a contactless sensor pad that is positioned under the mattress. It records minimal changes in pressure in real time. It records the movement data of patients or residents and helps to create an individual movement profile.
What role do aids play?
„An anti-decubitus mattress is a very important aid for people who are unable to change their lying position in bed independently,“ says the expert. Pressure-relieving mattresses, pillows and cushions are an integral part of modern pressure injury prevention.
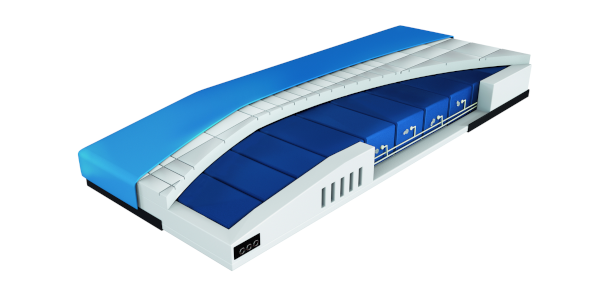
They support the body evenly and minimize pressure points. Such as the reactive mattress CliniCare 100 HF, which has a high-quality foam layer to relieve pressure points. If a compressor is connected, the support pressure can also be relieved using an alternating pressure mode.
However, Kolb warns against believing that such a mattress can replace repositioning. On the contrary: regular changes of position remain essential. The important thing is that the patient and their state of health should always be taken into account when deciding which aid is the most suitable. Misconceptions and ultimately bad purchases are quite common – because a 45-kilogram senior citizen with pressure sores needs a different support than a 120-kilogram patient with paraplegia.
Why are rubber rings and cushions unsuitable?
Rubber rings increase the pressure load on the side edges, which can lead to impaired blood flow. A soft cushion as a support in the wheelchair is well-intentioned, but gel cushions or soft padded cushions are more effective. The resulting support pressure is distributed evenly and pressure on certain areas is reduced. However, the seated position must also be monitored and limited in time. Wheelchair patients in particular, who are mobile thanks to their wheelchair, often disregard the one-sided pressure load and wounds develop.
How does skin care influence pressure injury prevention?
For centuries, the motto „smearing and ointment helps everywhere“ was common practice in pressure injury prevention. However, the expert standard „Decubitus prophylaxis in nursing care“ sees no connection between nursing care and pressure injury prevention. Rather, it is counterproductive to rub the skin with zinc or milking fat. This is because wounds remain permanently moist and heal poorly. Moisture from creams, sweating or incontinence even makes the skin more susceptible to pressure sores. Consistent cleaning, care and drying of the skin are therefore essential. It is better if professionals use skin protection products, especially water-oil emulsions. This is because they strengthen the skin’s natural protective film.
How does food affect the healing of wounds?
An appropriate diet significantly supports the healing process. It is important that breakfast, lunch and dinner contain sufficient proteins, vitamins, minerals and trace elements. It is also important for patients to drink plenty of fluids. Experts recommend at least 1.5 to two liters of fluid per day. However, it is important to note that is not the same as undernourishment. Even with a good BMI and a „healthy appearance“, a resident can be malnourished. Statistically, the risk of malnutrition is higher in older men than in older women. If you ignore healthy eating, you run the risk of pressure injury prevention failing.
Which old methods should be avoided?
Advice such as massage with rubbing alcohol is unsuitable for pressure injury prevention. The expert standard advises against care with alcohol. This dries out brittle skin even more. Expensive hydrocolloid plasters, which are often used for weeping wounds, also have no added value for pressure sores or other wounds.
Conclusion: Prophylaxis for pressure ulcers is a complex issue that always requires an individual approach tailored to the patient. Everyday routines must always be reviewed and adapted.


